Page 6 - RVO What Women Want May 2016
P. 6
6VV • What Women Want • An Advertising Supplement to the River Valley & Ozark Edition of the Arkansas Democrat-Gazette • Sunday, May 1, 2016
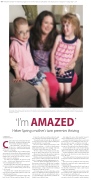
EILISH PALMER / CONTRIBUTING PHOTOGRAPHER Candyce Allen takes a break to sit with her 8-year-old twins, Kenneth and Chloe, at Allen Furniture in Heber Springs. The children were born at 25 weeks, along with their sister, Cara, who died at Arkansas Children’s Hospital in Little Rock at 10 1/2 months old. Allen and her husband, Greg, established the Cara Allen Diamond Award at the hospital for outstanding patient
and family-centered care.
‘I’m AMAZED’ Heber Springs mother’s twin preemies thriving
BY TAMMY KEITH SPECIAL SECTIONS WRITER
Candyce Allen’s twins celebrated their 8th birth- days April 21, and that was eight more than doctors told her the children would have.
Chloe and Kenneth — and Chloe’s identi- cal twin, Cara — weighed less than 4 pounds total when they were born. Cara never left the hospital
and died at 10 1/2 months.
Allen, 38, and her husband, Greg, 44, of Heber Springs
were married in 2004 and had trouble starting their fam- ily. She said an ectopic pregnancy damaged one of her Fallopian tubes, and the other was removed, so they de- cided to try in-vitro fertilization.
Two embryos were implanted. “We prayed a lot and it took — boy, did it take. My husband teases me that I don’t do anything halfway,” Allen said.
She had her first ultrasound on her 30th birthday, and the doctor told her she was pregnant with quadruplets.
“There were rays of sunshine coming out all over my body,” she said.
Greg hit the wall — literally. Allen said she heard a thud, and Greg had fallen back against the exam-room wall after he heard the news.
“I would just laugh because we had tried so hard to have kids,” she said. “This was a made-for-Lifetime-TV movie.”
It wasn’t the script she would have written, though. One of the babies stopped developing at eight weeks.
“It was hard because, at that point, we didn’t know if we were going to lose the others or what. Everything went smoothly until the 15-week checkup.”
The doctor told her that the girls had twin-to-twin transfusion syndrome — a disease of the placenta in which identical twins share a blood supply. “They said, ‘Your babies are probably going to die,’” she said.
“We were confused. Gosh, I think I cried for days. We tried to find as much support as we could,” she said. Allen went to Texas to have placental laser surgery, an
in-utero procedure for the twins, and it worked.
The babies started to grow and function as they should, but at 21 weeks, an ultrasound showed that she was di-
lated to 2 centimeters and had a bulging amniotic sac. “I had to lie with my feet higher than my head to re- lieve pressure off my cervix. I laid like that on complete bed rest for four weeks in UAMS. My only other option was to go to a hotel next to the hospital and wait it out. My whole thing is, as long as I knew I did everything I
could, I’m good with the outcome.”
At 25 weeks, almost to the hour that Allen said the
embryos were implanted, she knew something was wrong. Cara was about to be born, and Allen had to have a C-section immediately at the University of Arkansas for Medical Sciences Medical Center.
Cara weighed 15 ounces; Chloe weighed 1 pound, 5 ounces; and Kenneth was 1 pound, 10 1/2 ounces.
“I was pretty prepared because when you are in that situation, they do a lot of talking pretty early on to pre- pare you. They were tiny; you could see every vein — their skin was so thin — you could just see; everything was exposed. The girls had no hair; Kenneth had hair.”
“You ride that NICU roller coaster,” she said, referring to the neonatal intensive-care unit. After two weeks, the children were transferred to Arkansas Children’s Hospital.
“From the beginning, we knew Cara was having tough time. She was the sickest; she was septic when she was born,” Allen said.
“I drove back and forth to the hospital every day; Greg would come four times a week with me until Chloe came home.”
Chloe was 196 days old when she came home with a feeding tube, oxygen and a pulse-oxygen machine and several medications.
Kenneth, who had many brain bleeds, came home at 316 days with a tracheotomy, oxygen, a pulse-oxygen machine and a feeding tube.
“We knew Cara was sick, and we were told we would never bring her home. I think the staff, they held onto her as long as they could,” Allen said.
Cara was in the hospital 318 days when the decision was made to take her off a ventilator, and the family got